Maximilian Mai, CEO of the Memmingen Clinic, could actually look out of the window of his office at the landscape in the foothills of the Alps with satisfaction. Despite intense competition in the surrounding area, case volume at his hospital is high. Many patients value the facility highly and prefer it to other care options in the area because they feel they are in good hands, both medically and personally.
Internally, however, the management was repeatedly confronted with various challenges in the near past, particularly in the operating theater area. Thus, a significant number of the functional area’s employees terminated employment in a short period of time. The continued high number of surgeries threatened to overwhelm the capacity of the hospital and the remaining staff. In the search for the causes underlying this development, the clinic management encountered a diffuse and multi-layered problem situation. Inadequate OR capacity, poor communication, and hard-to-schedule work hours were frequently cited. Various possible solutions were put forward from all sides. These ranged from building new operating rooms, to reorganizing the OR, to recruiting new staff.
To prevent problems from becoming entrenched, the hospital decided to call on external support. At the end of 2019, Oberender AG, a management consultancy specializing in healthcare, will be commissioned to identify the underlying causes and find targeted solutions. “Some of the difficulties have grown historically and require a fresh start. For this, we rely on the combination of on-site know-how via our clinic director and the neutral view from the outside,” says Managing Director Maximilian Mai.

The Memmingen Clinic
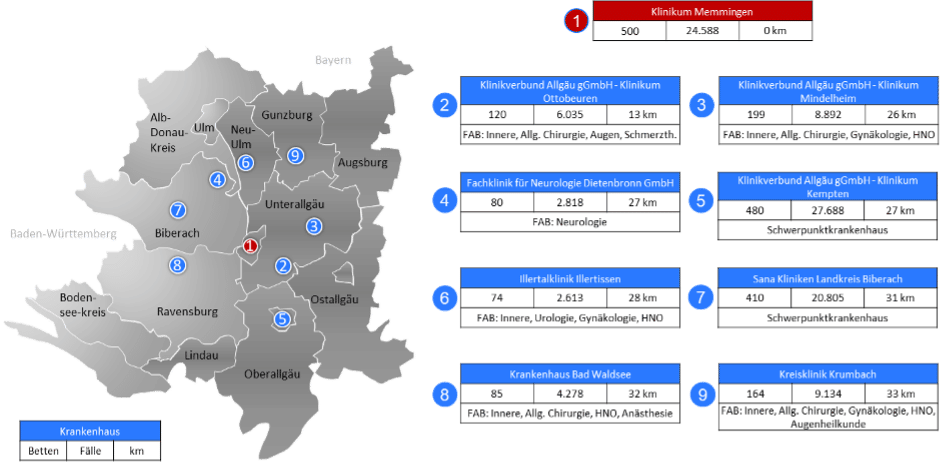
With its 1,800 employees and more than 500 beds, the hospital in Memmingen is of great importance in the region, both for the medical care of the population and as an employer. The 14 main departments of the priority care facility include the Clinic for General, Visceral, Thoracic and Vascular Surgery, Surgical Intensive Care Medicine and Pain Therapy, and the Clinic for Gynecology and Obstetrics. In 2019, 23,900 patients were treated as inpatients and 71,700 patients as outpatients. The teaching hospital of Ludwig Maximilian University in Munich enjoys an excellent reputation beyond the Allgäu region, which is reflected in a clearly supraregional patient catchment area despite intense competition (see Figure 1).
So far, the operating departments have included orthopedics and trauma surgery, general surgery, thoracic surgery, vascular surgery, gynecology, pediatric surgery, neurosurgery, urology and plastic surgery. In total, approximately 11,000 surgeries were performed in eight multidisciplinary ORs in 2019. The surgical wing is located in the old building of the complex, which leads to several challenges. Thus, separate discharge rooms, as found in newer OR buildings, are not present. Also, all the material needed for the operations must be stored in the operating room.
Challenges in the OR area
At the beginning of the mandate, a Quick Check will be conducted by Oberender AG in January 2020 to get a first overview of the OR area and the challenges. In this context, the first step is several visits, during which the consultants gain first-hand knowledge of the processes and structures as well as the hierarchies and communication channels. In addition, data is extracted and analyzed from existing clinical information systems and OR documentation.
The Quick Check makes it clear that a large number of fields of action exist. Optimizing OR planning is of central importance, as insufficient OR capacity results in various negative effects. The starting point here is the planning of the necessary capacities, which up to now has only been based to a limited extent on reliable key figures and the individual scope of the planned interventions. As a result, there are repeated peaks in workload, as a result of which the emergency operating room has to be used for elective procedures. In addition, excessively long lockout times and changeover times between ORs, as well as delayed OR starts in the morning, mean that elective procedures sometimes have to take place during the on-call period. All of these factors result in high employee stress, which is reflected in a high absenteeism rate due to illness of over 25% and the resignation of 16 of the OR’s 40 employees.
The next step of the Quick Check is to conduct employee interviews. This clearly shows that the employees have also recognized the need for change and are prepared to make it. Employees complain that the current procedure for OR planning and organization is not very transparent and thus not always comprehensible. On the part of the nursing staff, in addition to a stable OR schedule despite the high staff shortage and the number of emergencies, the desire for more appreciation of the work and for equal rights is expressed. For example, it is a recurring theme that the wishes of the various occupational groups are not taken into account equally in OR planning and that there is a hierarchy gap between the medical and nursing services. All employees are united by the desire “to be able to work in peace”.
Consulting by Oberender AG: Creating transparency through key figures
The results from the Quick Check show that changes need to be made primarily in the area of personnel as well as processes and structural conditions. In the area of personnel, the lack of employees and the hierarchical structures are particularly striking. The latter result not least from the fact that, in the absence of clear, data-based mechanisms for allocating the severely limited OR capacity, attempts are often made to resort to the law of the verbally stronger.
In the area of processes and structures, it shows that nearly 600 hours were overrun from core hours in 2019. Delays in the start of surgery are particularly common. For example, the first surgery in the morning in general surgery starts more than 18 minutes late on average. Since temporal variations in operations are partly due to differences in anesthesia conditions, these particularities must be taken into account in the analysis and in the implementation of changes. For example, for individual operations, it is necessary to check whether the anesthetic procedure is adapted to the operation and any deviations can be justified by an increased degree of severity in the patient clientele.
After identifying the problem areas in the OP, internal discussions began in March (see Appendix 1) about what changes were needed, in what areas, and by whom to address them. Right from the start, it became apparent that the debates were emotionally charged, which in some cases led to blockades. The consultants therefore initially initiated an OP working group to bring all the relevant professional groups to the table. It consisted of the chief physicians, the nursing director, the OR coordinator and the management. In this circle, a new OP concept was to be developed and implemented together with the consultants. To achieve this, it was essential that all employees pull together and support the changes. Clear communication rules have been established so that the concerns of each professional group are heard and any hierarchies have no influence. In addition, the working group always met with the same members in order to establish a personal level between the members and to ensure that information was consistently shared within the professional groups.
But even the newly formed working group alone could not effect change without having detailed information about performance in the OR. In addition, it became apparent that without this neutral data, it was also not possible to achieve a structured, targeted dialogue between the specialist and professional groups. Against this background, Oberender AG proposed to the Memmingen Hospital that it introduce a KPI-based OR management system with the aim of making the processes in the OR transparent and creating a factual basis for discussion.
The first step is an in-depth analysis of the data available within the clinic. Based on this, key figures were derived and developed and it was discussed which of the key figures should be included in the OR management system. At the same time, the results of the Quick Check already make it clear that although figures, data and facts must form the basis of a factual discussion, it takes many years of expertise to translate the resulting findings into operational recommendations for action and to implement these together with employees. For this reason, consultants from Oberender AG were used who themselves have many years of experience in the OR, for example as OR ward managers, and can therefore communicate at eye level with the various addressees.
General key figures
First, general key figures were developed that provide an insight into the work in the OR largely independent of the respective specialty groups and personnel types. The key figures are based on the “Glossary of perioperative process times and key figures: A Joint Recommendation of BDA/DGAI, BDC/DGCH and VOPM” of the relevant medical societies. In order to achieve the highest possible acceptance, care was also taken to use routine data as far as possible, i.e. data originally collected for documentation or billing purposes. In addition to the advantage that this procedure significantly reduces the effort required to collect data, the key figures compiled on this basis are particularly reliable and legally secure, as the respective documenters and management are liable for their accuracy.
In addition to the key figures in the glossary, further key figures are derived from the routine data:
- Ratio of table occupancy and cutting/sewing time
- By table occupancy: A room is considered to be at capacity when it is operated with 420 minutes of table occupancy time per day, 5 days a week, 50 weeks a year. In addition, there is 30 minutes of room-related preparation and follow-up time.
- According to cutting/sewing time: A hall is considered to be utilized if it is operated with 300 minutes of cutting/sewing time per day, 5 days a week, 50 weeks a year (delimitation according to Höhn).
- First cut times OP (collected in the course of further analyses)
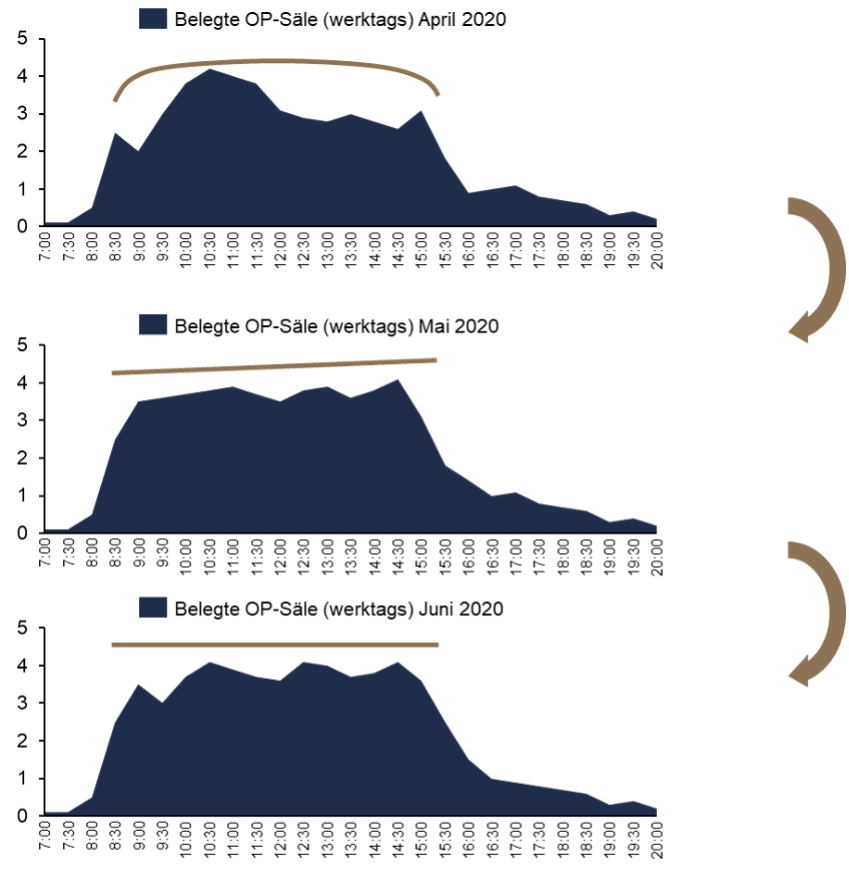
- Occupied operating rooms on weekdays
- Coating time: Display in minutes
Key figures per department
Individual problem areas were already particularly noticeable in the Quick Check, such as the fact that the surgeons in a specialist department frequently overrun the operating time or start late, resulting in disadvantages for the subsequent specialist departments in the operating schedule. However, the extent of such delays may be significantly distorted in the subjective perception of those who suffer. In order to create a transparent basis for argumentation and analysis in these areas as well, various key figures are therefore also derived from the routine data at the department level. These include:
- Utilization per department per month in % of available OR capacity according to DKI
- Deviation first cut in minutes per department
- Overrun time per department in minutes per month
- Overrun time in minutes per department without emergency indication
Introduction of a KPI-based OR management system
The metrics outlined in the previous section will be collected monthly and presented once a month at the Working Group OP beginning in May 2020. The individual departments are given room to justify negative deviations. For example, a high volume of complex treatment cases in a month may be a reason for longer than average surgeries. The extent to which this rationale is valid can be derived directly from the available data on the case severity of patients in a specialty department.
Following the introduction of KPI-based OR management, a key task was to address the problems identified in the area of personnel. The status quo of the hospital and thus also the problems should be made transparent for the employees through the preparation and presentation of the key figures. Employees are thus in a better position to understand the measures and the associated intentions and goals, which increased acceptance of the changes.
In addition, the OR management system should also serve to provide a foundation for all clinical staff to make informed decisions. Until now, physicians have not been able to independently access metrics and learn about performance events. Therefore, in collaboration with the internal controlling department, the data was processed and made available to the physicians in the form of a dashboard (see Appendix 2). Here, physicians can compile the information most important to them themselves and also make comparisons with other departments, for example with regard to OR utilization. With the introduction of the dashboard, it is now possible to reliably check one’s own gut feeling – for example, that other departments are overrunning their operating times more frequently. The occurrence of accusations is thus averted in advance.
At the same time, the key figures also show transparently in which areas other specialist departments are performing better. After the implementation of the dashboard, it often happens that the physicians of a specialist group independently initiate changes in view of the unfavorable and now transparent results for which they are responsible – for example, above-average OR turnaround times. External intervention is often no longer necessary. However, in order to be able to realize these positive developments in holdover times and delays in the entire OR area, it was necessary to fix this procedure in the processes and structures. To this end, physicians were held accountable for punctuality, which included adherence to surgery start and duration times, change times, and incision/suture times. As a result, surgeons, for example, have moved to ensure themselves that personnel are on site for the ensuing surgery and that there are no delays.
Results of the OR reorganization
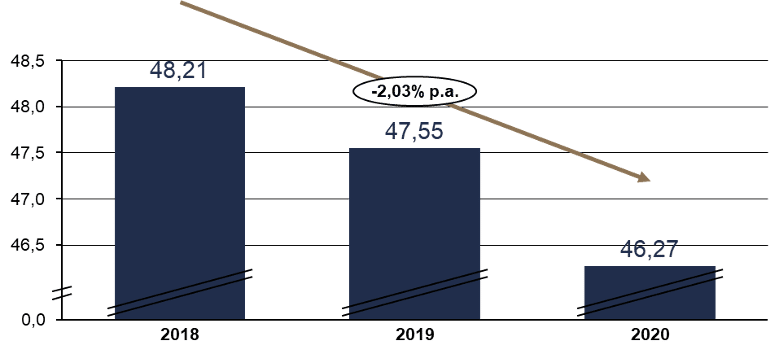
Following the introduction of the KPI system, positive developments can be seen in the area of processes. The changeover times can almost always be reduced in the individual halls. Even though it increases slightly in room 2, the decrease is significant on average (see Figure 2). The cutting/sewing time is also reduced almost across the board.
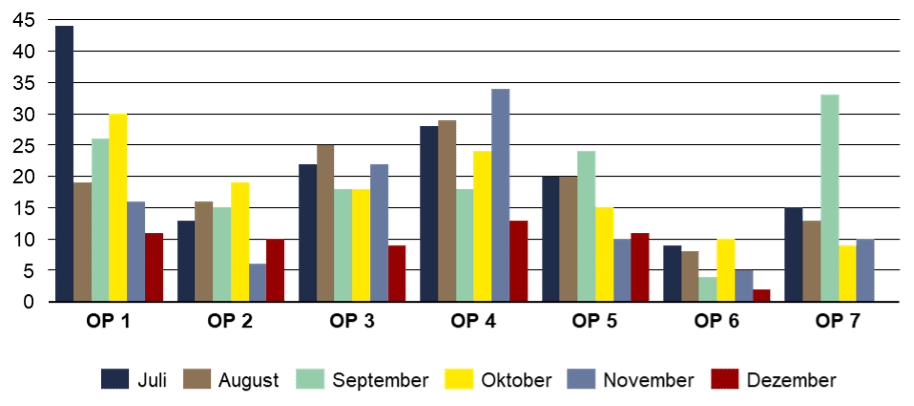
The changed processes and responsibilities additionally contribute to the positive development of the deviations of the first cut and the overrun time per department over time (see Figures 3 and Appendix 4). The reduction of the deviation of the first cut can be observed especially in OP 1 and OP 5. The November outliers in OP 4 are due to a higher than average number of emergencies and comparatively complex cases causing delays.
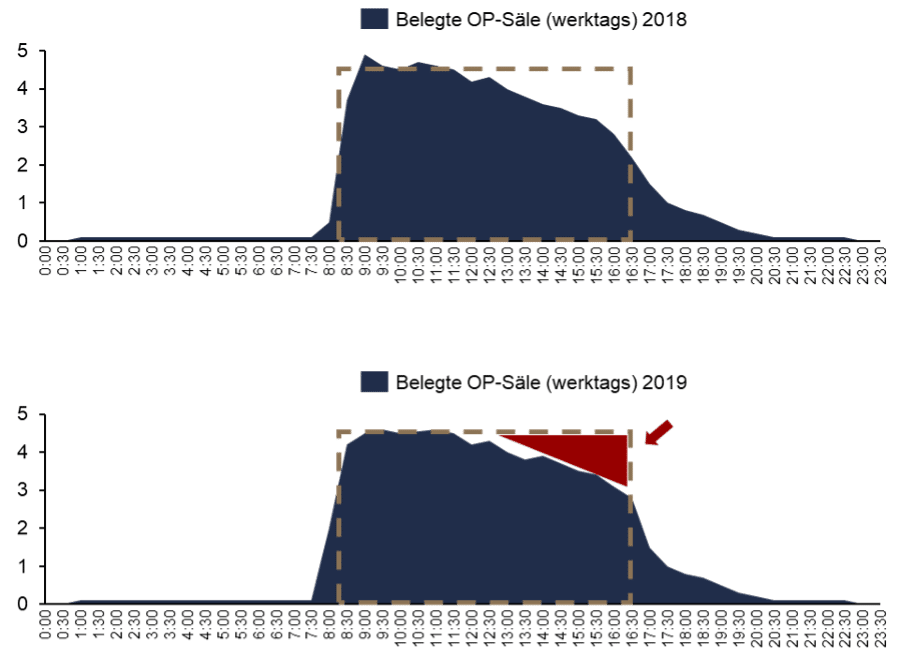
Overall operating room utilization has been optimized by improving processes, making the initial cut earlier, making utilization more consistent, and making the room end on time. Thus, the number of concurrently running auditoriums has compressed in terms of time and increased in terms of occupancy (see Figure 4). Significant progress was made towards the goal of utilizing as many halls as possible during the core working hours (red triangle) so that there are no overruns or vacancies.
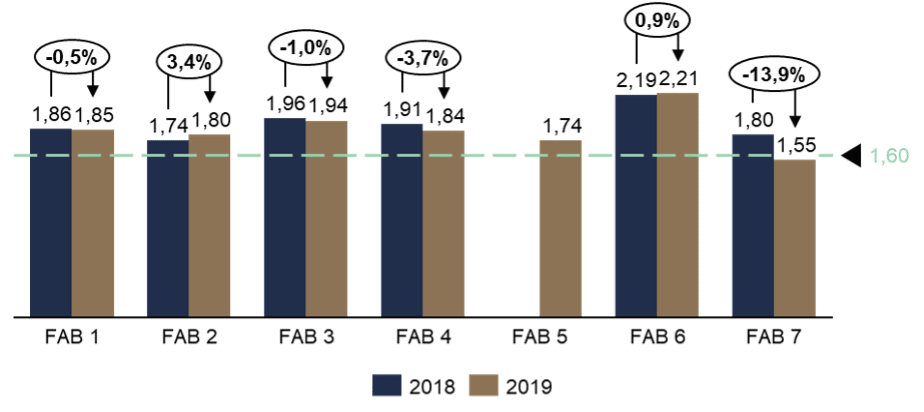
At the department level, it can be seen that ORs are increasing in the large departments and decreasing in the small ones. A closer approximation to the 1.6 factor of anesthesia to incision suture time was achieved in most departments (see Figure 5). The improvements achieved during the consultation process, such as more punctual start dates and shorter handover times, are partly responsible for this.
Satisfaction is expressed by the staff after the restructuring. Employees feel comfortable and valued. Interdisciplinary agreements have also increased, for which the OR dashboard provides a factual basis for discussion. The significant reduction in unplanned operating day extensions and the resulting decrease in overtime also played a key role in increasing employee satisfaction. It is noteworthy that all these improvements were realized despite a slight increase in the number of cases and during the high additional burden of the Corona pandemic.
Nest Steps
At the end of 2020, the hospital’s management is very satisfied with the results achieved: The diffuse problem situation at the beginning of the year, for which no direct solution was yet apparent, was not only transparently presented, but largely resolved. From the perspective of the clinic management, the changed working atmosphere, which is characterized by appreciation and professionalism, shows that the measures and changes have contributed to a sustainable improvement. This has not only led to a reduction in the number of redundancies, but has even made it possible to recruit new skilled workers. “A start has been made, we have achieved a lot this year, especially in the personnel situation. However, we are not yet at the end of the optimization process, but we want to continue to strongly involve the employees in the further processes in any case,” says Management Board member Maximilian Mai.
The many process optimizations that have been implemented on the basis of the transparent data situation have also resulted in significant efficiency gains. This has resulted in a decrease in the need for operating room capacity and nursing staff despite a slight increase in the number of cases. The construction of additional operating rooms, which seemed inevitable even before the start of the consulting mandate, was thus averted. The freed-up funds can be used for other important projects, such as the expansion of the digital infrastructure or the renovation of the operating theater discharge area.












