No matter how different they are, all municipalities in Bavaria are affected by the massive upheavals in the healthcare system. 90 out of 96 districts or independent cities are directly responsible for a hospital, two others are at least indirectly involved. This means that almost everyone who is responsible in a municipality is confronted with seriously changing framework conditions and high financial risks and burdens.
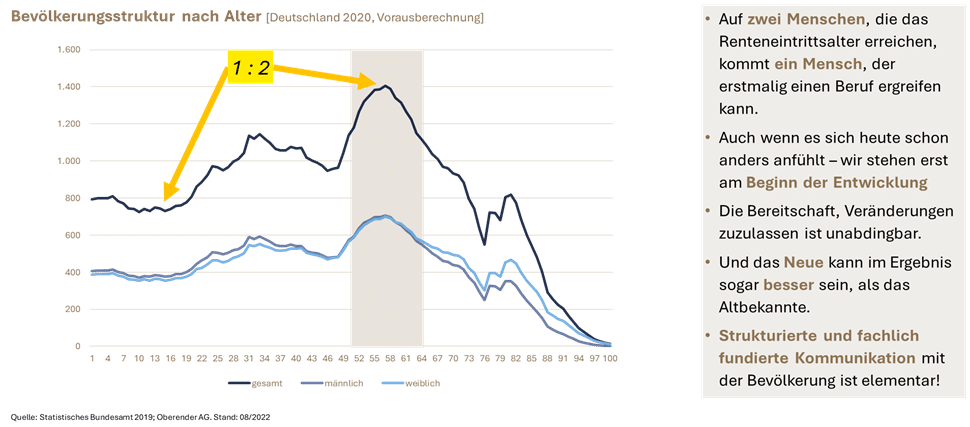
No matter what you think of the political decisions in Berlin, the real drivers of change are different: Medicine is becoming ever more efficient, but also places ever greater demands on infrastructure, the availability of a wide range of specialists and comprehensively qualified personnel. At the same time, we are only at the beginning of an even more acute shortage of skilled workers: for every two people who reach retirement age, there is one who can enter a profession.
Demographics will shape our area of activity in the coming years.
In addition, the financial reserves of both the health insurance funds (also due to the increasing number of pensioners who pay lower contributions than those in employment) and the federal government (weak economy, beginning repayment of special funds) have been exhausted.
In addition to the high density of municipal hospitals, Bavaria has another special feature: 54% of all hospitals in Bavaria have fewer than 150 beds. At the same time, the beds are only utilized to an average of 60 to 70 %. However, 100 occupied beds are no longer sufficient by the standards of modern medicine (apart from specialist clinics) to make good medicine economically successful.
As a rule, they can no longer meet the minimum requirements for the infrastructure necessary for emergency care (e.g. for the treatment of strokes or heart attacks). This means that the emergency departments of many of these hospitals already have the problem that they can no longer adequately treat the most serious emergencies. Instead, more and more minor injuries and illnesses are being treated that do not actually require the expensive infrastructure of a hospital.
High-quality emergency care is essential
However, this is still often perceived differently by the general public. It assumes that the local hospital is the best solution for good emergency care, while at the same time moving to larger and more specialized facilities for planned interventions. It is much more important (and often no less challenging) to create structures in the rescue service that allow patients to be reached in the shortest possible time and transported to the nearest suitable facility. The nationwide provision of these suitable facilities must be ensured.
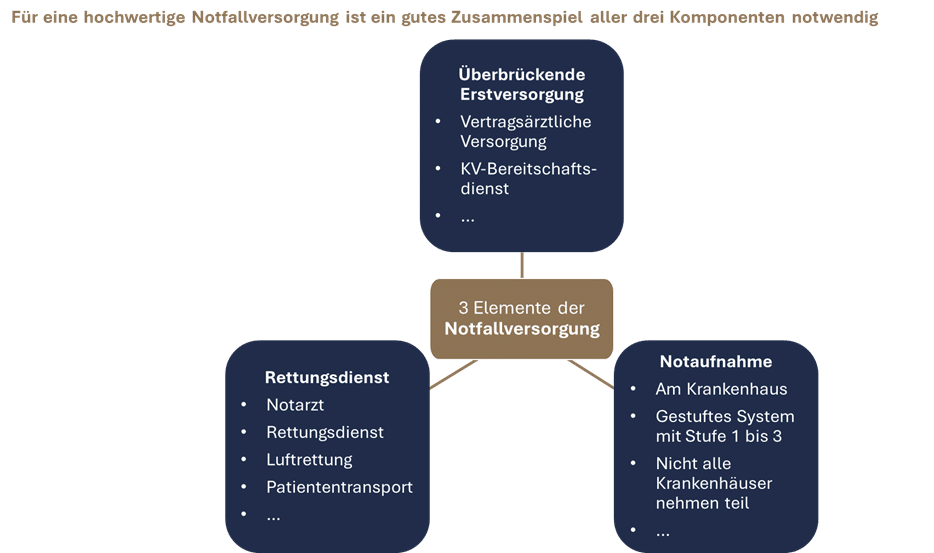
It is therefore quite possible that a small location in a region will have to be significantly expanded in order to be able to provide emergency care, while at the same time two smaller locations will have to be closed or converted to provide a different range of care.
However, the room for maneuver of many municipal hospital operators is now significantly limited. In the past, they have made many investments and offset deficits. But the district levy is under pressure, the coffers are empty and the financial supervisory authority is threatening. While other mandatory municipal tasks can only be carried out with difficulty and often no longer satisfactorily, large sums of money flow into the local hospital. And as things stand at present, the deficits of hospitals in Germany will continue in the medium term – the hospital reform will not begin to take effect until 2027 at the earliest with regard to new remuneration approaches (advance remuneration), and there is no prospect of an interim law to reduce deficits. On the other hand, structural requirements are increasing and driving costs up further.
Waiting is not an option.
Every operator must critically question today what it can and wants to achieve financially over the next ten years and what future prospects its hospital has – irrespective of its own financial capacity. And even if the local authorities are responsible for ensuring inpatient care, this does not mean that a hospital is needed in every district or independent city. The question needs to be expanded accordingly: What will medical care in the area look like in the future (perhaps even without inpatient capacities) in one’s own district or independent city? Medicine should be where it is needed, which does not necessarily have to coincide with the location of a hospital. “Digital before outpatient before inpatient” is a common, if not always trivial to implement, paradigm that addresses this issue.
In the area of inpatient care, the introduction of service groups with structural requirements and the expansion of hybrid DRGs will further accelerate previous downward trends. What is needed is a sober analysis of the status quo and possible development paths in both medical and economic terms.
Key questions for further development
- What is the current state of emergency care in the region? Can guideline-compliant care be provided in all relevant areas?
- Which areas of the hospital can be maintained medically in the long term, and which will no longer meet the requirements?
- Where does the house stand economically? What other municipal tasks are possible subsidies in competition with?
- What development options are there for the hospital (strengthen and expand the location, renovate the location economically, convert the location into alternative services, etc.)?
- What does outpatient care look like today and tomorrow, and what role does the hospital play in it?
- Can emergency care be provided (possibly even better than in the status quo?) without the hospital? What changes might be necessary in the rescue service, what services would be desirable in bridging first aid?
- Aus welchen Bausteinen kann eine zukunftssichere, ambulant-stationäre Versorgung zusammengestellt werden und wie kann die Umsetzung erfolgen?
- Etc.
However, three aspects appear to be of particular importance:
- The toolbox of different measures and instruments for designing new care structures has expanded massively in recent years and is getting bigger with every reform.
Cross-sector care providers / level 1i hospitals are now to be able to emerge from hospitals that continue to maintain a small bed management unit but otherwise primarily perform outpatient tasks. Health regions, health kiosks and pilot systems are further keywords that conceal possible solutions. In-depth technical expertise is required in order to make a serious assessment of the opportunities and limitations specific to the region. - In-depth technical expertise is required in order to make a serious assessment of the opportunities and limitations specific to the region.
If this is not communicated and the population and local stakeholders are not involved, the most sensible initiatives regularly fail or are delayed for so long that the small window of opportunity in which it would still have been possible to intervene in a creative way closes. Communication must master both worlds: Broad-based communication, but also an understanding of the context so as not to raise false expectations or promote unfounded fears. - From the local authority’s point of view, it needs to be carefully considered what role it can and wants to play in shaping the supply structures. This includes a realistic consideration of the extent to which skills and time resources are available to get involved in the topics. The complexity of the healthcare system is almost impossible to grasp, even for experts, because inpatient and outpatient services are regulated too differently and the legal requirements are too heterogeneous. At the same time, the local authority’s influence is extremely limited, much is decided by the local government or other stakeholders and the local authority can only formulate requests and wishes. But there are also many possible lines of political conflict. It does not always make sense to be at the forefront of implementation – sometimes others can simply do it better, sometimes there is simply no really good option.
So just pessimism everywhere? Certainly not!
The next few years will undoubtedly be challenging and many tough decisions will have to be made. However, we must not forget that one reason for this change is the many new possibilities that medicine offers us today, but which were not even foreseeable when the structures that exist today were formed. There is every reason to hope that we will continue to receive better medical care in the future. What will change, however, are the structures in which medicine is provided. The self-responsibility of the population and patients will also play a role, as will the new distribution of responsibilities between different healthcare professions and the use of new technological possibilities.
However, the prerequisite for this is to become active.
The window of opportunity to actively shape the future, at least to a large extent, is limited. Once a hospital is close to or already in insolvency, the scope for action is extremely limited. A domino effect is set in motion, as staff are hard to recruit and reputations – whether justified or not – are damaged. Municipalities are therefore obliged to think through all eventualities at an early stage, especially in the interests of the population. Even an uncomfortable path in the short term can be the right one in the long term. Very often, the analysis will also show that the hospital location is actually indispensable and only the orientation needs to be adapted to the current circumstances.
Recommendations for further reading
On the transformation of hospital sites: Rhön Foundation brochure for local decision-makers
On intersectoral health centers, the source of ideas for the cross-sectoral care providers now envisaged in the KHVVG: Two expert reports commissioned by the KBV
On primary care centers: Brochure of the Robert Bosch Stiftung
Remark
This article appeared in the publication Landkreistag KOMPAKT, issue no. 5/2023.
Jochen Baierlein gave a presentation on “Successful medical area coverage” at the 54th District Councillors’ Conference on October 11, 2023. This is the detailed article.
















