Classification of nursing in the economy
The health care sector is one of the largest labor markets in Germany. In 2012, it had 5.2 million employees. Trade journals refer to the healthcare industry as a job and employment engine, because it is growing more than the rest of the economy. In 2017, it already counts 5.6 million employees with a share of women of 75.8% and a share of employees over 59 years of age of 11.6%. A comparison with the automotive industry confirms the importance of the healthcare sector for the labor market in Germany. With a turnover of 376 billion euros in 2017, the healthcare industry is at a similar level to the automotive industry, which achieved a turnover of 423 billion euros in 2017. However, by contrast, the automotive industry only had around 820,000 employees in 2017. This means that the number of employees in the healthcare sector is around seven times higher than in the automotive industry
Aim and purpose
“Of the nursing workforce, 770,000 were registered professionals in 2018, according to the Federal Labor Relations Authority. From 2017 to 2018, there was an increase of 21,200 (2.8%) registered nurse professionals. Accordingly, registered nurse professionals accounted for 13.8% of all healthcare workers in 2017.
Due to the high significance of hospital nursing for the labor market in the Federal Republic of Germany and the often discussed economization of the hospital sector, we would like to approach the question of economization of hospital nursing with this report. What does economization actually mean? What numerical facts worth knowing are available to us? What is the importance of nursing care for a hospital? We would like to find answers to these questions in this report. We begin with the question of economization.”
What does economization actually mean?
Economy (economy) is understood as the totality of all actors, which are connected with each other in a certain context. Examples are the economy of a country, a family or even a company. In terms of content, it concerns, for example, their endowment with resources (labor and capital), their interactions with each other and the results thereof. All economies face the circumstance of resource scarcity. With respect to health care, health economics deals with the economic analysis of the health care system. As part of this analysis, health economists answer questions such as:
- Are resources being allocated correctly and according to need?
- Is the treatment of diseases carried out at the lowest possible cost with a given level of quality, or are resources wasted?
Health economists refer to the first question as the allocation problem. In economics, allocation means the distribution of scarce resources or production factors (labor, capital) to different needs. Economization has also arrived in the hospital. What has happened?
Economization in the hospital
In Germany, the SGB V § 71 stipulates the principle of contribution rate stability. This means that the agreements on remuneration between service providers and payers must be designed in such a way that increases in health insurance contribution rates are excluded as far as possible. In accordance with Section 12 of the German Social Code, Book V, services must also be adequate, appropriate and economical. They must not exceed what is necessary. In order to comply with these principles, policymakers introduced a new reimbursement system in the early 1990s that focused on promoting the efficient use of resources. Prior to this measure, per diem care rates, without reference to the treatment effort for individual patients, did not provide an incentive for efficient use of resources in hospitals. The new reimbursement system, which was introduced across the board in the hospital sector
Diagnosis Related Groups (DRGs)
In DRGs, highly simplified groups are formed for diagnoses or treatments that cause a similarly high economic expenditure of resources. For each of these groups, the average expenditure incurred across all hospitals is determined. From this, cost ratios of the individual DRGs are formed (relative weights). These are multiplied by the so-called state prime rate. The result is a monetary amount per case of treatment (DRG), regardless of the hospital in which the treatment is provided. This is therefore a payment based on average costs. As of 2004, billing via DRG charges was mandatory for all somatic hospitals. Since then, revenues via DRG charges have been based on the average costs of hospitals. The size of one’s own margin compared to the margin of other hospitals now results from the relative cost structure. The resulting incentives are, for example, to optimize one’s own cost structure or the provision of services. Implementing these economic constraints strategically is also necessary in many hospitals, because investments increasingly have to be financed from operating income. In the next section, we will examine key figures related to hospital care.
Compilation of interesting facts, figures and data
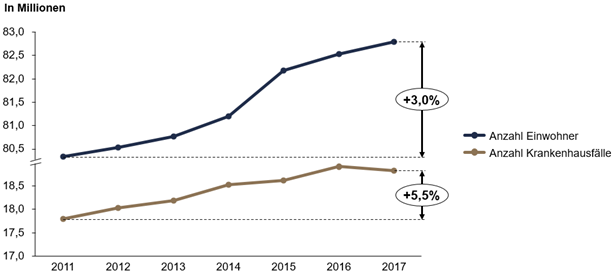
A look at the following Figure 1 shows that the population in Germany has grown by a total of 3.0% between 2011 and 2017. During the same period, the number of hospital cases has also increased, but by 5.5%.
As mentioned above, the healthcare sector is one of the largest labor markets in Germany. The central factor influencing why the healthcare sector, but also the social sector, is one of the largest growth and economic drivers in Germany is demographic development. An excerpt from the 14th coordinated population projection (Table 1) shows, based on the basic assumption of a relatively old population, that the number of very old people will increase by 35% from 2018 to 2060, while the number of people of working age will decrease by 24% in the same period:
| Jahr | Anzahl hochbetagter Menschen (Alter: über 67-jährige) | Anzahl erwerbsfähiger Menschen (Alter: ab 20 bis 66 Jahren) | Summe hochbetagter und erwerbsfähiger Menschen |
| 2018 | 15,9 Millionen | 51,8 Millionen | 67,7 Millionen |
| 2060 | 21,5 Millionen* (+35%) | 39,4 Millionen (-24%) | 60,9 Millionen (-10%) |
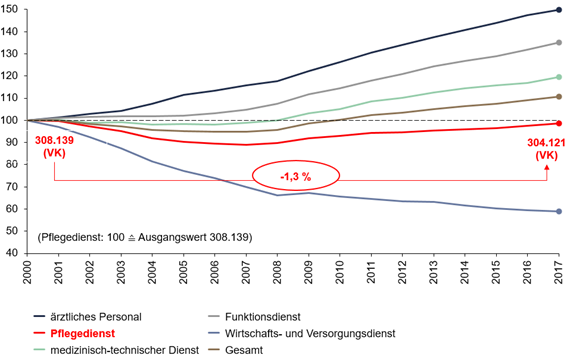
The following Figure 2 illustrates that between 2000 and 2007, i.e. precisely during the period when flat rates per case were introduced, there was a decline in the number of full-time nursing staff in hospitals. Since 2007, the number of nurses has been increasing again, but there has still been an overall decrease of 1.3% in full time nurses from 2000 – 2017.
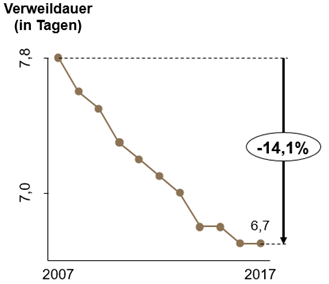
Furthermore, it should be noted that the length of stay in hospital has been decreasing almost continuously since 2007. The following Figure 3 shows that in 2007, a patient was hospitalized for an average of 7.8 days; in 2017, by contrast, the average is only 6.7 inpatient days per patient. Accordingly, the length of stay fell by a total of 14.1% between 2007 and 2017.
At the same time, the discussion mostly assumes an increased workload in the form of a service compression in the hospital. This is justified, as shown in the following table 2, with the increased number of cases to be cared for per full-time employee in the nursing service from 2003 to 2015, which has increased by 12%.
| Jahr | Anzahl zu versorgenden Fällen je Vollkraft (VK) im Pflegedienst* |
| 2003 | 57 |
| 2015 | 64 (+12%) |
Furthermore, as part of the Hospital Barometer 2019, prepared by the German Hospital Institute (DKI), 268 general hospitals in Germany were surveyed about vacant or unfilled positions in the nursing service. Extrapolation to the population of all general hospitals with 100 beds or more shows that around 12,000 full-time positions on general wards in the nursing service were unfilled in 2019. In 2016, 3,900 unfilled nursing service positions are assumed, which is about a three-fold increase in vacant nursing positions. This trend is also evident in critical care staffing. In 2016, there were still 3,150 unfilled positions. In 2019, there were already 4,700 unfilled positions in critical care. This represents an increase of around 50%. In the fact check nursing staff in hospitals from 2017, various study results are shown, in the context of which the future development of nursing staff was examined. For example, Ostwald et. al. (2010) and Rothgang, Müller and Unger (2010) assume a range of between 400,000 – 490,000 vacancies in hospitals, preventive and rehabilitation facilities and nursing homes for the year 2030. In contrast, the study by Afentakis and Maier (2010) forecasts a number of vacancies in nursing occupations of 152,000 for the year 2025. What is the importance of hospital nursing and why is qualified nursing staff so indispensable?
Importance of nursing in hospitals
The German Federal Ministry of Health (BMG) makes it clear that safe and good treatment of patients in hospitals is only possible with good nursing staffing levels. For this reason, nursing staff sublimits will apply in four nursing-sensitive areas (intensive care, geriatrics, cardiology and trauma surgery) from January 2019. These nursing staff sublimits have not only been tightened as of January 2020, but also expanded to include additional areas. The nursing staff sublimits are set as the maximum number of patients per nurse. For example, in geriatrics, a nurse may care for a maximum of ten patients during the day shift (06:00 – 22:00), and a maximum of 20 patients per nurse during the night shift (22:00 – 06:00). Hospitals that do not adhere to the guidelines and fall below the limits must accept reductions in remuneration or even case numbers. Due to the corona crisis, the lower nursing staff limits were suspended by the German Federal Ministry of Health (BMG) in spring 2020, and are now to be gradually reinstated.
Care-sensitive areas
“Nursing-sensitive areas in hospitals are, in the sense of the legislator, those areas in which, from the point of view of patient protection as well as from the point of view of quality of care, there is a correlation between the number of nursing staff and the occurrence of adverse events, such as a pressure ulcer or an infection of the surgical wound (so-called “nursing-sensitive outcome indicators”). This means that nursing-sensitive hospital areas are vulnerable to adverse events to the extent that they are understaffed.” Initial indications of nursing-sensitive areas are based on an expert report by the Hamburg Center for Health Economics (hche) dated Nov. 16, 2016 (Schreyögg expert report). What do we take away for the future?
Findings and outlook
Compared with the automotive industry, the healthcare sector employs seven times as many people for a similar turnover. This sector of the economy is one of the largest labor markets in Germany. Of the total number of employees in the healthcare sector, registered nurses accounted for around 13.8% in 2017. Due to demographic developments, the demand for healthcare services will increase, while the number of people capable of working will continue to decline. This will also have a greater impact on nursing services in hospitals; it is already noticeable. Furthermore, statutory nursing staffing requirements are increasingly being extended. Those who do not comply with the specifications will be sanctioned. From an economic point of view, qualified nurses are already a scarce resource that must be used wisely. The fact is: without well-trained nursing staff, medical services cannot be provided in hospitals. The performance of an operation or the care of critical patients in intensive care units are just two examples. It is also necessary to ask how qualified personnel can be optimally deployed in the future in the face of increasing demands. This is where Paracelsus Medical Private University comes in, for example, with its master’s degree program in nursing science. Fields of activity and framework conditions must be created in the future for the highly qualified graduates of such courses.




